We are currently in the midst of an enormous crisis associated with pain-relieving opioid drugs such as morphine, heroin, and the now infamous oxycodone (sold as ‘OxyContin’).
To give a sense of the scale of this crisis, from 1999 to 2017 the US experienced a 600% increase in opioid-related deaths, and recent estimates indicate that over 600,000 people have died from opioid overdoses across North America over the last 20 years1-3. In 2020 alone, more than 70,000 Americans and 6,000 Canadians died from an opioid overdose – a number that has likely increased each year since1,3.
How did this happen?
Ironically, it was predominantly driven by well-meaning doctors who wanted to relieve their patients of their chronic pain. But why did doctors think it was alright to prescribe opioids to their patients at a large scale? To answer this, let’s briefly walk through the history of opioid prescribing.
During the second half of the 20th century, chronic pain was increasingly identified as a highly prevalent yet under-treated condition1. Although opioids were long recognized as powerful analgesic (‘pain-relieving’) drugs, they were only reserved for extreme forms of pain associated with cancer or surgery. This is because they were long acknowledged for their addictive potential and potential for harm. However, around the 1980s, on the basis of what now seems to be shoddy evidence and over-interpretation1,3, a subset of doctors began to question this conventional wisdom. These doctors claimed that opiates were non-addictive when prescribed for the treatment of pain and that they can be safely used for this purpose.
At the same time, influential US organizations such as the American Pain Association and The Joint Commission began strongly advocating for the need for adequate assessment and treatment of pain. This led to pressure on doctors and health care organizations to provide effective pain treatments. Moreover, this pressure was compounded by the fact that US organizations are allocated federal funds based on patient satisfaction. It goes without saying that chronic pain patients that were prescribed opioids were typically more satisfied (at least in the short term) than those that were not – so this created even more incentive for liberal prescribing.
Seeing this opportunity, pharmaceutical companies began heavily marketing opioid drugs – often paying doctors to advocate for the safety and efficacy of their products despite a lack of reliable supportive evidence. Most notably, in the mid-90s a company called Purdue Pharma introduced a sustained-release version of an opioid drug (oxycodone, trade name ‘OxyContin’) which they claimed was less addictive. To quote an article from Nature, in order to market their product, “[Purdue Pharma] lobbied lawmakers, sponsored continuing medical-education courses, funded professional and patient organizations and sent representatives to visit individual doctors. During all of these activities, they emphasized the safety, efficacy and low potential for addiction of prescription opioids”. This was a huge success: from 1997 to 2002, OxyContin prescriptions increased from 670,000 to 6.2 million4.
Turns out, OxyContin is highly addictive and Purdue Pharma knew it – they eventually admitted it in a 2007 lawsuit and had to pay a $635 million USD fine5. Later, in 2020, they also admitted to fraud and two other felony offenses. Finally, earlier this year (2022), more justice was served, and the family that owns Purdue Pharma was ordered to pay as much as $6 billion USD to pay for damages to individuals and communities as a result of their role in the opioid crisis.
We need changes.
The fact that OxyContin was approved by the US Food and Drug Administration and trusted by doctors across North America despite being based on fraudulent claims should ring alarms for many. It reveals the critical (and seemingly unmet) need for reliable regulatory bodies which operate independently of the pharmaceutical industry, and which rigorous evaluate drug safety and efficacy in the absence of conflicts of interest. It also signals the need for effective independent monitoring of drug safety after regulatory approval – something that has been left to shady pharmaceutical companies in the past. There are also many other issues highlighted by this catastrophe – check out this in-depth article by leading experts to dive deeper.
In the end, chronic pain is indeed a highly prevalent and sometimes debilitating condition that requires effective treatment.
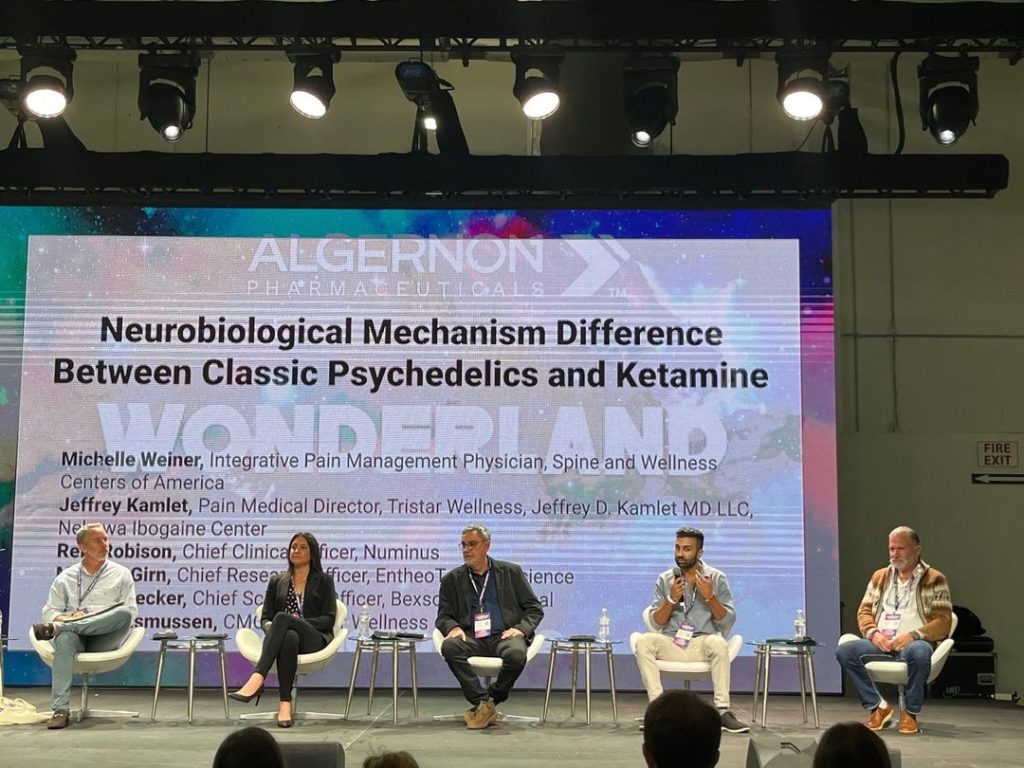
The development of less addictive but effective drugs and holistic, integrative interventions is sorely needed. This is where drugs such as ketamine, or serotonergic psychedelics such as a psilocybin, may play an important role. It is our belief that these two drugs – embedded within a biopsychosocial holistic framework – have significant potential to play a role not only in reducing symptoms of chronic pain, but also in helping individuals to overcome their opioid addiction. At the least, we sincerely hope that they pave a way forward away from excessive dependence on opioids as a treatment option for chronic pain.
References