In a highly influential and much-discussed 1977 paper in the prestigious journal Science, American psychiatrist George L. Engel highlighted the limitations and flaws of the dominant model for treating psychiatric diseases¹. This dominant model — which is still the most influential today — is the biomedical model of mental illness. In essence, this model proposes that mental illness can be completely reduced to biological dysfunctions in your brain, usually at the level of brain chemistry. It downplays or ignores completely the role of other factors in the patients’ life, and provides treatments that are based on rectifying these biological changes, usually in the form of a pharmaceutical drug.
As a counter to this approach, Engel outlined what he calls the biopsychosocial model. As the name suggests, this approach involves a holistic, systems-level perspective on mental health which acknowledges the interacting influences of biological, psychological, and social factors. It highlights that a given illness for a given individual may require a greater focus on one or another of these other factors, rather than a single-minded focus on biology. The approach of this model seeks to re-humanize psychiatry and highlight the unique ways that a given illness can be triggered, expressed, and interpreted by a given individual in a particular sociocultural context. It also involves more of a participatory role for the patient in the psychiatrist-patient relationship, where their personal subjective experiences and perspectives play a greater role in diagnosis and treatment selection.
Although it’s been over 40 years since Engel introduced this model — and although it has certainly made a positive impact and facilitated changes in standard medical approaches² ³ — the biomedical model is still largely the dominant framework in psychiatry. For example, if you’ve read our previous blog posts on ketamine, you’ll very quickly realize that the biomedical model constitutes the standard approach to ketamine in medical contexts, whereas the biopsychosocial model is more in line with the framework of ketamine-assisted therapy (KAT).
In particular, the biomedical approach to ketamine devalues and ignores the experience elicited by ketamine, as well as the unique personal history and social embeddedness of the patient, and highlights its effects on the structure and chemistry of the brain. Whereas, the biopsychosocial approach of KAT — which our EntheoMed Ketamine Assisted Therapy Suite upholds — is a holistic and patient-centered approach that highlights the often highly personal nature of the ketamine experience and the many non-biological factors that relate to the individual’s illness and its treatment.
You might ask: how is it that the biomedical model has persisted when clearly a biopsychosocial approach seems more apt to deal with the complexities of the human experience? There are of course a whole variety of factors that contributed to this, but one important historical factor comes to mind. During the second half of the 20th century (including when the biopsychosocial model was proposed), psychiatry was going through an identity crisis. This crisis revolved around whether psychiatry is truly a medical discipline or whether it is more so to be viewed as an extension of psychology. This question arose largely because, as a result of the complexity and (by definition) subjective nature of mental illness, psychiatry struggled to reach the scientific standards that were present in other fields of medicine, particularly with respect to diagnosis. In this context, with the creation of the standardized and symptom-based DSM diagnostic system and the discovery that brain chemistry altering drugs can relieve symptoms, psychiatry jumped on the opportunity to uphold a wholly biological conception of illness that was on par with the rest of medicine⁴⁵. This need for acceptance as a medical discipline came at the cost of excluding the ‘messiness’ of psychological and social factors.
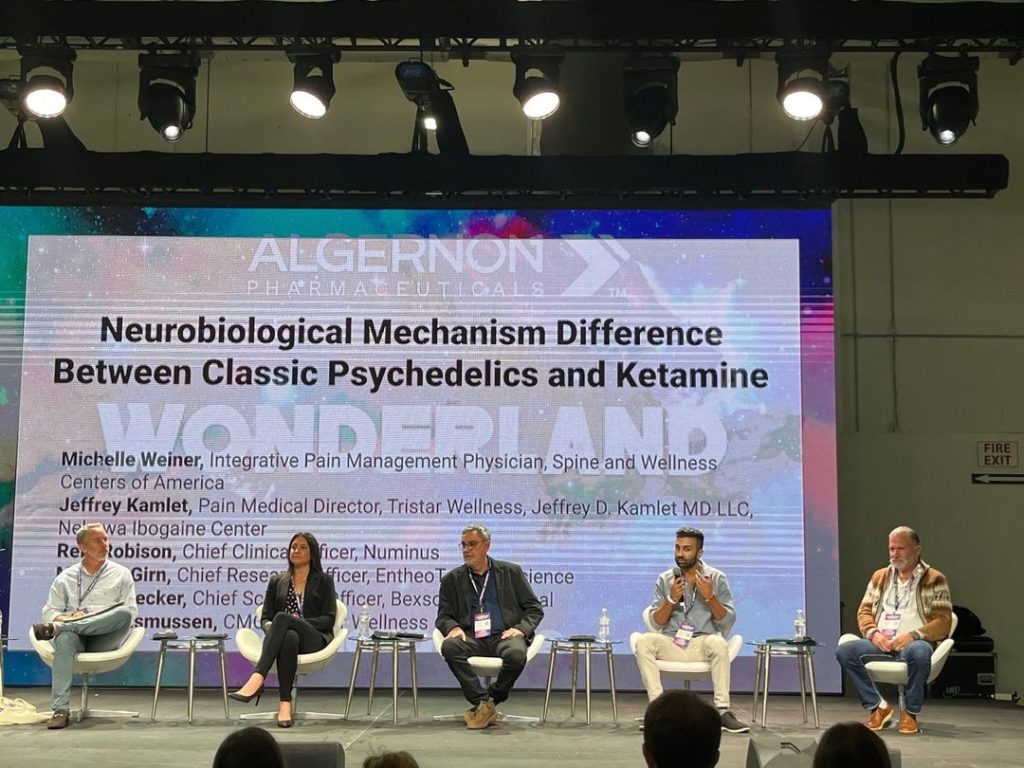
Times are changing, however, and one can argue that the increasing mainstream acknowledgement of the efficacy of psychedelic and ketamine assisted psychotherapy is playing a major role in both highlighting the limitations of the biomedical model, and of showing the need for more holistic and patient-centered biopsychosocial approaches. Time will tell how much longer the biomedical hegemony will last.
Written by Manesh Girn for EntheoTech
REFERENCES
(1) The Need for a New Medical Model: A Challenge for Biomedicine
(3) The Biopsychosocial Model 25 Years Later: Principles, Practice, and Scientific Inquiry
(4) “Shrinks, The Untold Story of Psychiatry,” by Jeffrey Lieberman, MD